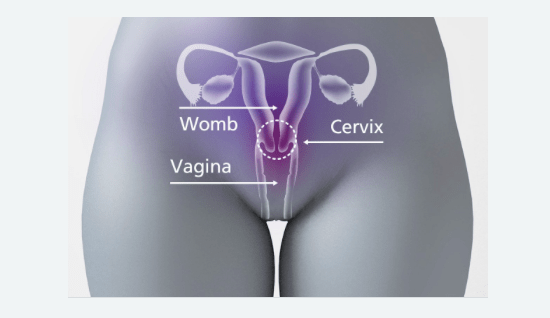
Cervical cancer is a cancer anywhere in the cervix, the opening between the vagina and the womb (uterus), also known the neck of the womb.
It is a leading cause of mortality among women. It is estimated that over a million women worldwide currently have cervical cancer and most of them have not been diagnosed, nor do they have access to treatment that could cure them or prolong their lives.
- In 2020, 604 000 women were diagnosed with cervical cancer ;
- 342 000 women died from the disease;
- It is the most commonly diagnosed cancer in 23 countries and is the leading death cause in 36 countries. Many of these countries are in sub-Saharan Africa, Melanesia, South America, and South-Eastern Asia.
Even though all countries are affected, the incidence is higher in low- and middle-income countries and the proportion of women with cervical cancer who die from the disease is greater than 60% in many low- and middle-income countries, which is more than twice the proportion in many high-income countries, where it is as low as 30%. This discrepancy of cervical cancer incidence and mortality in low- and middle-income countries are not attributable to differences in cervical infection with oncogenic HPV types. Instead, they are mainly attributable to the relative lack of high-quality cervical cancer screening and lack of widespread high-quality treatment of invasive cervical cancer in those countries.
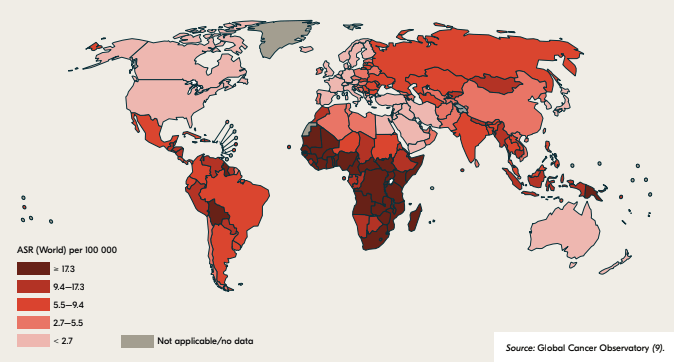
group, 2020
The global burden of this clinical condition is projected to continue to increase, rising to 700 000 cases and 400 000 deaths in 2030, representing a 21% increase in the number of cases and a 27% increase in the number of deaths over just the 12-year period from 2018.
This situation is a consequence of decades of neglect by the global health community. However, with the recent rise in global advocacy for women’s health, availability of prophylactic vaccines, low-cost approaches to screening and treating cervical cancer precursors, development of resource-appropriate management guidelines, novel approaches to surgical training, and initiatives to increase global access to anti-cancer drugs, there is still hope of changes.
HPV AND CERVICAL CANCER
The primary cause of pre-cancerous and cancerous cervical lesions is the infection with a high-risk or oncogenic Human Papilloma Virus (HPV) type. HPV are very common group of viruses (more than 100 types) of which at least 14 cause cancer. A subset of HPV types is responsible for virtually all cases of cervical cancer. The most oncogenic types are HPV 16 and 18, which together causes about 70% of cervical cancer worldwide.
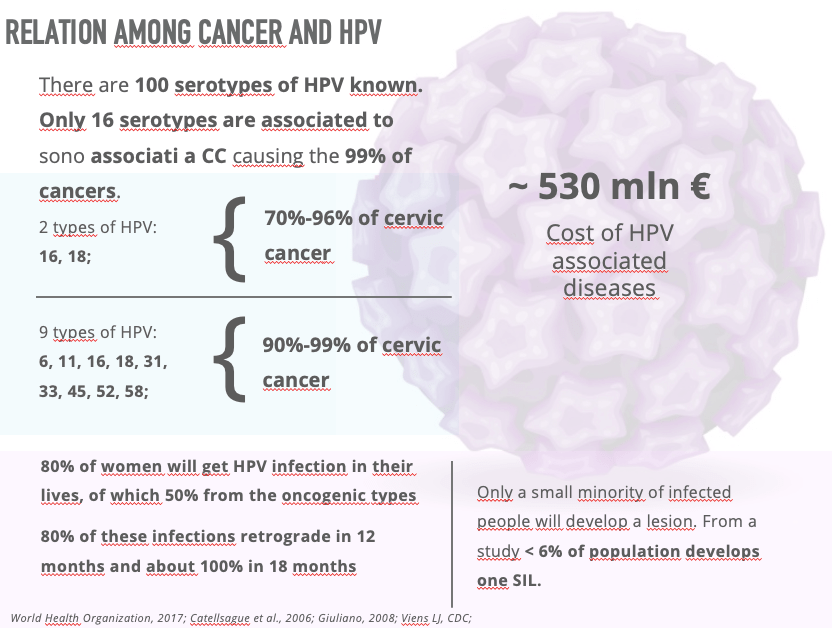
Cervical HPV infection is a commonly, and mostly sexually transmitted infection and pathogenesis is the same worldwide. Other causes are skin to skin contact of the genital area, vagina and oral sex and sharing sex toys. Other factors can be involved in the transmission and epidemiology.
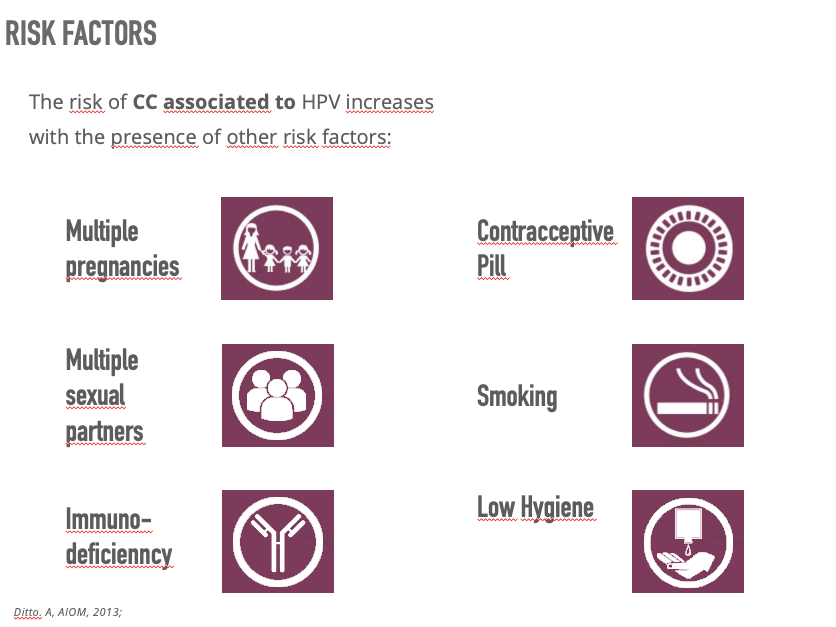
Anyone with a cervix can get cervical cancer: women, trans-men, non byname people and intersex people with cervix. You might also be more likely to get cervical cancer if you are under 45 , you have a weakened immune system (HIV , AIDS,…), you have given birth to multiple children or had children at an early age, your mother took hormonal medicine diethylstilbestrol while pregnant and you had vagina, vulva, kidney or bladder cancer in the past.
Infection with certain HPV types also causes a proportion of cancers of the anus, vulva, vagina, penis, and oropharynx, which are preventable using primary prevention strategies like those for cervical cancer.
Sign and Symptoms of cervical cancer include:
- Unusual vaginal bleeding
- Change to your vaginal discharge
- pain during sex
- pain in you lower back, between your hip bones or lower tummy
It is impossible to always prevent cervical cancer but there are things you can do to lower your chances like:
- Regular screening for women between the ages of 25 and 64 in order to treat any changes in the cells of the cervix before they can turn into cancer
- HPV vaccine to all children aged 12 to 13
- Using condoms
- Quitting smoking
- Eating a balance diet
HIV AND CERVICAL CANCER
Cervical cancer is the most common cancer among women living with HIV, having a risk several times higher of persistent HPV infection, six times as likely to develop cervical cancer and women are more likely to develop it at a younger age.
Despite the gains in prolonged life expectancy associated with access to HIV care and treatment, cervical cancer in women living with HIV has not received the attention and resources that are needed to address its prevention and treatment, and screening coverage has often been low. Reaching vulnerable women at high risk of developing cervical cancer and acquiring HIV infection will need prioritization of integrated preventive, screening, and treatment services for both diseases to increase efficiencies and maximize impact.
PREVENTION AND STRATEGIES
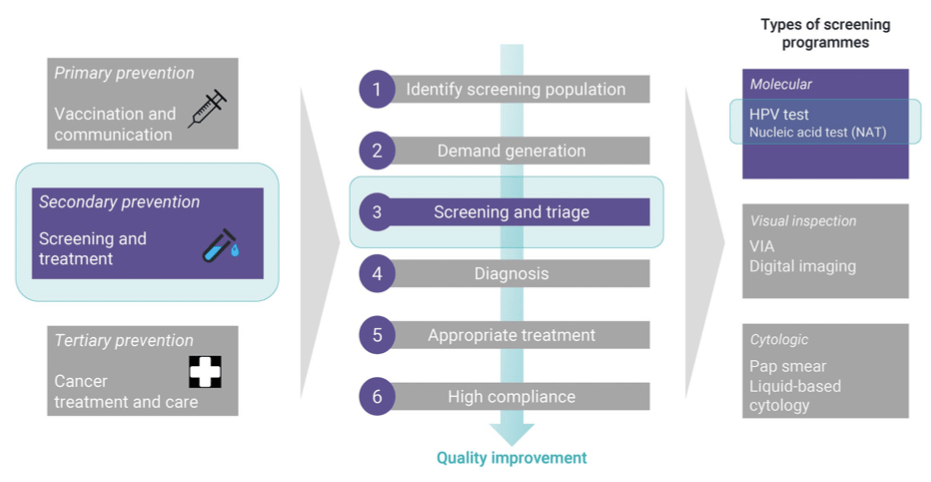
Since 2007, WHO has recommended a comprehensive, life-course approach to prevention and control of cervical cancer, which has formed the basis of the move towards elimination of this condition.
In May 2018, Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization (WHO), issued a call to action for the elimination of cervical cancer. A WHO global strategy to accelerate the elimination of cervical cancer as a public health problem was presented and unanimously endorsed by the Seventy-third World Health Assembly in August 2020. The Global Strategy states that to reach the elimination threshold of four cases of cervical cancer per 100 000 women a year by the end of the century, countries should reach the following targets by 2030 (the “90–70–90” targets) and maintain them from that point on.
The targets of the global strategy are, by 2030:
• to vaccinate 90% of eligible girls against HPV.
• to screen 70% of eligible women at least twice in their lifetimes; and
• to effectively treat 90% of those with a positive screening test or a cervical lesion, including palliative care when needed.
In the context of this global strategy, countries are updating their protocols for the prevention of cervical cancer and for the care and treatment of affected women. Cervical cancer prevention also plays an integral role in reaching the Sustainable Development Goals (SDGs), both for health (SDG 3) and gender equality (SDG 5).
CERVICAL CANCER CONTROL INTERVENTIONS
What interventions we have to protect ourselves to develop cervical cancer?
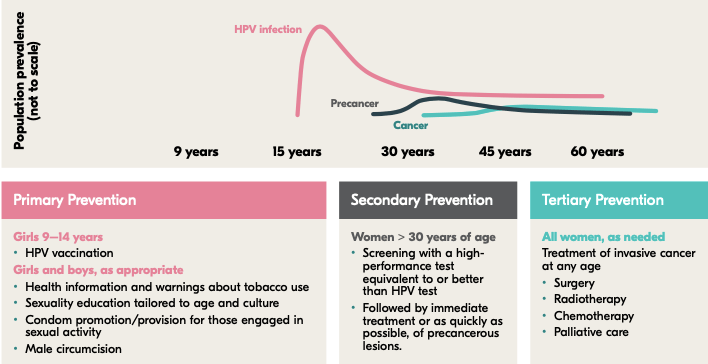
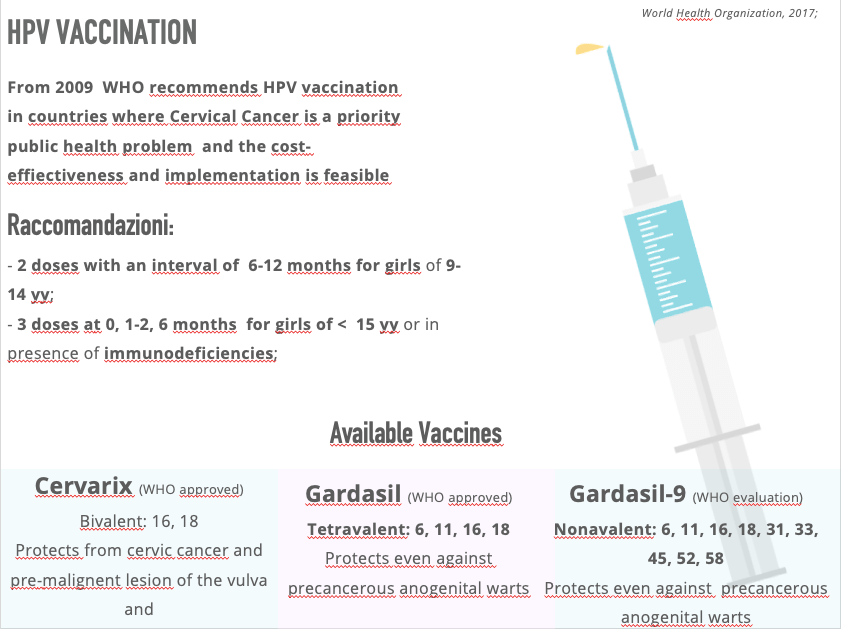
PRIMARY INTERVENTION: HPV VACCINATION
Between 2006, when the first HPV vaccine was licensed, and 2017, more than 100 million adolescent girls worldwide received at least one dose of HPV vaccine, 95% of whom were in high-income countries. Access to HPV vaccination is improving, and in 2019 more than 65% of the girls being vaccinated each year globally were living in low- and middle-income countries.
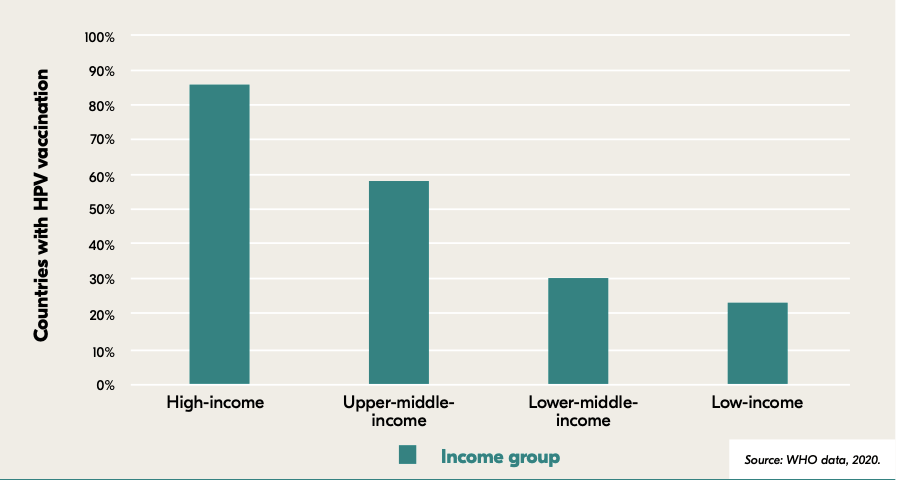
As of 2020, less than 25% of low-income and less than 30% of lower- and middle-income countries had introduced the HPV vaccine into their national immunization schedules, while more than 85% of high- income countries had done so.
Vaccination of adolescent girls is the most effective long-term intervention for reducing the risk of developing cervical cancer. The great long-term benefit of HPV vaccination makes it important to initiate and sustain this approach in all countries. There is also strong evidence that high HPV vaccination coverage leads to protection of unvaccinated individuals through herd immunity, further enhancing the protective effect for the community. WHO’s current guidelines recommend that young adolescent girls between 9 and 14 years receive two doses of vaccine to be fully protected.
In addition to HPV vaccination, it fundamental to have an age-appropriate information and communication on sexual and reproductive health, safer sexual practices, and cessation of tobacco use.
SECONDARY PREVENTION: SCREENING AND TREATING PRECANCEROUS LESIONS
The principal goal of the secondary prevention is to reduce cervical cancer incidence and mortality by identifying and treating women with precancerous lesions. A cervical intraepithelial neoplasia (CIN) is characterized by cellular changes in the transformation zone of the cervix. It is typically caused by HPV high-risk types such as strains 16 and 18. CIN1 lesions (low-grade squamous intraepithelial lesions) are morphological correlates of HPV infections. CIN2/3 lesions (high-grade squamous intraepithelial lesions) are correlates of cervical pre-cancers, that if left untreated, may progress into cervical cancer. These lesions can be identified using various tests, selecting those who have or are at risk of cervical pre-cancer.
Three approaches to cervical cancer screening and future tests
| Molecular | Cytologic | Visual inspection |
| Nucleic acid amplification tests (NAAT)a » high-risk HPV DNA/ NAAT » mRNA DNA methylationb Protein biomarkersb » HPV antibodies » oncoproteins | Conventional Pap smeara Liquid-based cytology (LBC)a Dual staining to identify p16 and Ki-67a | Visual inspection with acetic acid or with Lugol’s iodine (VIA/VILI)a » naked eye » magnified by colposcope or camera Automated visual evaluation of digital imagesb |
a Current tests
b Tests under evaluation (future tests).
The traditional method to screen women for cervical cancer is the cytology method (the Papanicolaou test, also known as the Pap smear or smear test). When cytology results are positive, the diagnosis is confirmed by colposcopy, and then biopsy of suspicious lesions for histological diagnosis. Newer screening tests introduced in the last 15 years include visual inspection with acetic acid (VIA), and molecular tests, mainly high-risk HPV DNA-based tests, which are suitable for use in all settings. More recently, other newer tests and techniques have been developed:
- other molecular tests such as those based on HPV mRNA
- oncoprotein detection or DNA methylation;
- objective tests performed on cytological samples such as p16/Ki-67 dual staining;
- advanced visual inspection tests based on artificial intelligence/machine learning platforms (e.g. automated visual evaluation of digital images).
Testing for HPV offers superior specificity, and its strong negative predictive value means that women who test negative only need to be retested after a minimum interval of five years. Providing women with the option of self-sampling contributes to acceptability and access to services.
INVASIVE CANCER TREATMENT AND PALLIATIVE CARE
Timely assessment and referral of women with suspected or confirmed cervical cancer are crucial for saving lives and preventing disability. Comprehensive management of invasive cervical cancer requires well-equipped, appropriately qualified health providers and access to pathology, medical imaging, surgical, radiotherapy and chemotherapy services.
Management of each case is based on staging the disease. Early-stage cervical cancer is highly treatable by surgery and/or radiotherapy, which can result in long-term survival and/or cure. The five-year survival rate for early-stage cancer is more than 80% in countries where timely diagnosis and high-quality treatment are available. Surgery and radiotherapy, with or without chemotherapy, are among the cost-effective interventions that WHO recommends for early-stage cervical cancer. Even some locally advanced cervical cancers are curable with high-quality concurrent chemoradiation.
Palliative care can be integrated into the treatment plan and provided throughout the course of the disease. There can be some treatment-related effect as bladder dysfunction, bowel dysfunction, sexual dysfunction, lymphoedema and psychosocial problems. It is very important to consider them to guarantee a good quality of life of eomen cancer. In addition to managing pain and other distressing symptoms, care should involve psychosocial and spiritual support for women and their families.
In conclusion….
Bold strategic actions are needed to eliminate cervical cancer and to improve community awareness. In order to ensure optimal effectiveness, these actions must be developed in concert with front-line health care policymakers and providers, advocates, and women themselves. Furthermore, development of workforce capacity, strengthening of national health systems, shaping the market to lowering the prices of life-saving products, accelerating the introduction of affordable technology into screening and treatment algorithms, organizing population-based prevention and treatment platforms are other key elements that all countries, especially the middle- and low-income countries, need to take in consideration for the sake of all women.
REFERENCES
- “Global strategy to accelerate the elimination of cervical cancer as a public health problem” World Health Organization 2020
- “Introducing and scaling up testing for human papillomavirus as part of a comprehensive programme for prevention and control of cervical cancer- a step by step guide” World Health Organization 2020
- “WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention, second edition” World Health Organization 2021
- “Comprehensive Cervical Cancer Control A guide to essential practice Second edition” World Health Organization 2014