April is the Caesearn awareness month and we are here to give you simple and useful insights about this topic in order to be able to make the best decision .
The World Health Organization recommends that caesarean section be performed only when medically necessary.
Some data:
- In 2012, about 23 million C-sections were done globally.
- The international healthcare community has previously considered the rate of 10% and 15% to be ideal for caesarean sections.
- Some evidence finds a higher rate of 19% may result in better outcomes.
- More than 45 countries globally have C-section rates less than 7.5%, while more than 50 have rates greater than 27%.This obviously reflect of the possibility for some places to be easier to access to some services.
- In general, then caesarean sections have become increasingly common in both developed and developing countries for a variety of reason, with governments and clinicians have expressed concern about the rise in the numbers of caesarean section births and the potential negative consequences for maternal and infant health
But before talking about the social, cultural and economical impact of the ceaseran section, we want to give you a simple explanation about this procedure.
BACKGROUND

A caesarean section, or C-section, is an operation to deliver your baby through a cut made in your tummy and womb. The cut is usually made across your tummy, just below your bikini line.
It’s a major operation that carries a number of risks, so it’s usually only done if it’s the safest option for you and your baby.
A caesarean may be recommended as a planned (elective) procedure and done from the 39th week of pregnancy, or done in an emergency if it’s thought a vaginal birth is too risky. It may be carried out because:
- your baby is in the breech position (feet first) and unable to be turned by applying gentle pressure to your tummy, or you’d prefer they did not try this
- you have a low-lying placenta (placenta praevia)
- you have pregnancy-related high blood pressure (pre-eclampsia)
- you have certain infections, such as a first genital herpes infection occurring late in pregnancy or untreated HIV
- your baby is not getting enough oxygen and nutrients – sometimes this may mean the baby needs to be delivered immediately
- your labour is not progressing or there’s excessive vaginal bleeding
If there’s time to plan the procedure, your midwife or doctor will discuss the benefits and risks of a caesarean compared with a vaginal birth.
ASKING FOR A CAESAREAN
Some women choose to have a caesarean for non-medical reasons. The decision should be discussed with your midwife and/or a doctor, to consider both the benefits and the riskS to you and your baby compared with a vaginal birth.
If after discussing all the risks and hearing about all the support on offer you still feel that a vaginal birth is not an acceptable option, you should be offered a planned caesarean. If your doctor is unwilling to perform the operation, they should refer you to a doctor who will.
It is normal and understandable to be anxious and scared in giving birth, nobody is born ready (even though the society thinks like that) but any mental and wellbeing support should be given by an healthcare professional.
WHAT HAPPENS?
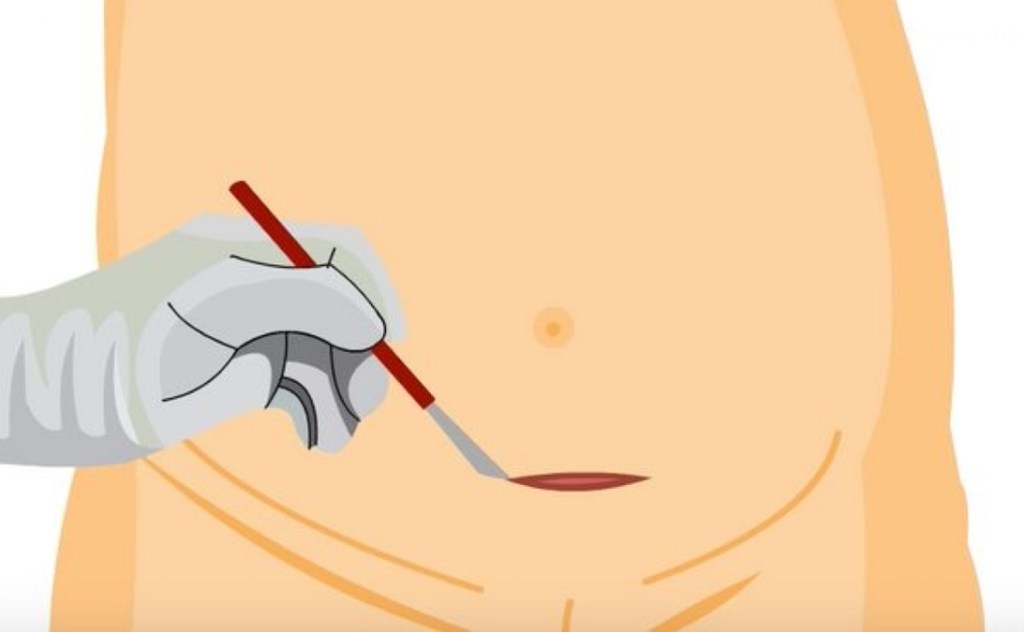
Most caesareans are carried out in hospitals and they will perform a spinal or epidural anesthetic. This mean you’ll be awake, but the lower part of your body is numbed so you will not feel any pain. Obviously before the operation, exams and blood test will be performed to understand if there are any clinical conditions to be aware.
During the procedure:
- a screen is placed across your body so you cannot see what’s being done – the doctors and nurses will let you know what’s happening
- a cut about 10 to 20cm long will usually be made across your lower tummy and womb so your baby can be delivered
- you may feel some tugging and pulling during the procedure
- you and your birth partner will be able to see and hold your baby as soon as they have been delivered if they’re well
The whole operation normally takes about 40 to 50 minutes.
Occasionally, a general anesthetic (where you’re asleep) may be used, particularly if the baby needs to be delivered more quickly
RECOVERY
The avarage stay in hospital after a caesarean is around 3 or 4 days, where you and the baby will be takig care. During these days it is very important to create a close contact with the baby and start to breastfeeding.

Even though you might feel pain, you will be encouraged to drink, eat and thought how to take care of your wound after you will be at home ( clean and dry every day, wear loose clothes, take pain killers if needed and monitor any sign infections). The operation will leave eventually an horizontal scar just under your tummy, that will probably hidden by pubic hair (in darker skin the scar tissue may fade to leave a brown or white mark)
Most women experience discomfort the firts few days after the operation as pain, bleeding. Discuss with your doctor the type of painkillers you can take and consider to use sanitary pads for heavy bleeding.
Is usually adviced to move and do gentile activities, in order to speed up the recovery and reduce the risk of blood clots. But maybe before 6 weeks after you get home you won’t be able, because not safely yet, to do:
- driving
- exercising
- -carrying anything havier than your baby
- having sex
Always ask your midwife and gp if you are unsure when it is safe to start returning to you normal activities.
WHEN TO GET MEDICAL ADVICE

A caesarean section is generally a very safe procedure, but like any type of surgery it does carry a risk of complications. The level of risk will depend on things like if the procedure is planned or carried out as an emergency, and your general health condition. Contact your midwife or a GP straight away if you have any of the following symptoms after a caesarean:
- severe pain
- leaking urine
- pain when peeing
- heavy vaginal bleeding
- your wound becomes more red, painful and swollen
- a discharge of pus or foul-smelling fluid from your wound
- a cough or shortness of breath
- swelling or pain in your lower leg
These symptoms may be the sign of an infection or blood clot, which should be treated as soon as possible.
Risks to you
Some of the main risks to you of having a caesarean include:
- infection of the wound (common) – causing redness, swelling, increasing pain and discharge from the wound
- infection of the womb lining (common) – symptoms include a fever, tummy pain, abnormal vaginal discharge and heavy vaginal bleeding
- excessive bleeding (uncommon) – this may require a blood transfusion in severe cases, or possibly further surgery to stop the bleeding
- deep vein thrombosis (DVT) (rare) – a blood clot in your leg, which can cause pain and swelling, and could be very dangerous if it travels to the lungs (pulmonary embolism)
- damage to your bladder or the tubes that connect the kidneys and bladder (rare) – this may require further surgery
Women are now given antibiotics before having a caesarean, which should mean infections become much less common.
Risks to your baby
A caesarean can sometimes cause the following problems in babies:
- a cut in the skin (common)
- breathing difficulties (common) – this most often affects babies born before 39 weeks of pregnancy; it’ll usually improve after a few days and your baby will be closely monitored in hospital
If you think your baby is having breathing difficulties after you have left hospital, see a GP or call your national emergency number
Risks to future pregnancies
Women who have a caesarean usually have no problems with future pregnancies and can have a safely vaginal birth, called vaginal birth after caesarean (VBAC).
Although uncommon, having a caesarean can increase the risk of certain problems in future pregnancies, including:
- the scar in your womb opening up
- the placenta being abnormally attached to the wall of the womb, leading to difficulties delivering the placenta
- stillbirth
SPECIAL SITUATIONS
- In Judaism, there is a dispute among the pokism(Rabbinic authorities) as to whether the first-born son from a caesarean section has the laws of a bechor (The role of firstborn son carries significance in the redemption of the first born son, in the allocation of a double portion of the inheritance, and in the prophetic application of “firstborn” to the nation of Israel).
- In rare cases, caesarean sections can be used to remove a dead fetus; otherwise, the woman has to labour and deliver a baby known to be a stillbirths
- The mother may perform a caesarean section on herself; there have been successful cases, such as Inés Ramírez Pérez of Mexico who, on 5 March 2000, took this action. She survived, as did her son, Orlando Ruiz Ramírez.
Refernces
1- https://www.nhs.uk/conditions/caesarean-section/
2- Molina, G; Weiser, TG; Lipsitz, SR; Esquivel, MM; Uribe-Leitz, T; Azad, T; Shah, N; Semrau, K; Berry, WR; Gawande, AA; Haynes, AB (1 December 2015). “Relationship Between Cesarean Delivery Rate and Maternal and Neonatal Mortality”. JAMA. 314 (21): 2263–70. doi:10.1001/jama.2015.15553. PMID 26624825
3- “WHO Statement on Caesarean Section Rates”(PDF). 2015. Archived (PDF) from the original on 1 May 2015. Retrieved 6 May 2015.
4- See Chok Yaakov 470:2; Kaf ha-Chayim 470:3; “Archived copy”. Archived from the original on 18 August 2010. Retrieved 28 July 2010
5- “Pidyon HaBen — Definition of Pidyon HaBen (Redemption of the Firstborn)”. Judaism.about.com. 19 October 2012. Archived from the original on 19 October 2011. Retrieved 15 August 2011
6- “Kohanim forever from the sources, who is a cohen, the blessing of the Cohanim,. Mitvah of the cohen, Halacha, Temple service groups, pidyon—redemption of the firstborn”. Cohen-levi.org. Archived from the original on 18 August 2011. Retrieved 15 August 2011
7- Casey, Francis E. “Elective Abortion”. Medscape. Medscape. Archived from the original on 14 December 2004. Retrieved 18 March 2016